Accutane is a medication prescribed to treat severe and stubborn cases of acne that hasn’t responded to standard acne treatments.
And since fungal acne is notorious for its resistance to standard acne treatments, some people believe that Accutane may be their best option to get rid of this challenging condition once and for all.
Therefore, if you are considering getting on Accutane to get rid of fungal acne, there are a few things you need to know before making a final decision.
In this article, we’ll explore the effectiveness of Accutane for fungal acne and offer some alternative treatments that may be worth trying.
What is Fungal Acne, and What Are the Symptoms?
Fungal acne is is a skin condition where Malassezia yeast begins to grow in the hair follicles, which has a similar appearance to traditional acne.
The symptoms of fungal acne are similar to traditional acne with a few key differences:
- Fungal acne is typically itchy
- Fungal acne typically appears in small clusters
- Fungal acne is more common on the back, chest, and arms, although it can appear anywhere
- Fungal acne usually manifests itself in the form of small pustules, and while they can also look like “closed comedones” without a white head on the tip sometimes, they are never cystic or larger than just a dot.
- Fungal acne is accompanied by excess dandruff
Another tale-tell sign that you’re dealing with a case of fungal acne is breaking out from pretty much everything you apply on the skin, including serums, moisturizers, and most frequently, sunscreens. Because of this we recommend checking the ingredients of all your skincare products in this fungal acne ingredient lookup tool.
These are pretty much all the warning signs of fungal acne, so besides taking them into consideration and visually comparing your affected areas to Google photos, there’s only so much you can do to identify them without professional assistance. Because of this we recommend setting up a dermatologist consultation if you believe you may have fungal acne.
This will involve a trip to the doctor’s office where your health provider would perform a shave biopsy by scraping the flared-up areas and sending the sample to a lab.
Another, more accurate way to determine your condition is to have a microbiologist extract a comedone and analyze the DNA by using a real-time PCR system and a quantitative PCR reagent.
What Causes Fungal Acne?
Fungal acne or Malassezia folliculitis is caused by an inflammatory reaction to Malassezia yeasts.
Pityrosporum or Malassezia are yeast species present in an estimated 92% of the world’s population as part of the skin microbiome.
This tells us that the skin can be free from pimples even while the yeast lives on it. So, the issue has to be something else than just the yeast causing problems for absolutely no reason.
Well, as it turns out, there could be several factors that could turn this usually commensal (neutral) yeast into an opportunistically harmful pathogen.
Here are some potential causes of fungal acne:
Internal Factors
It has been observed that there are higher incidences of fungal acne among patients with diabetes, HIV, Hodgkin’s disease, as well as those with nutritional disorders and immunologic deficiencies.
Another common trigger factor can be the prolonged use of broad-spectrum antibiotics due to their ability to alter the gut microbiota and skin flora, causing the yeast to proliferate.
However, the main factor of Malassezia overgrowth in healthy individuals seems to be an overly rich sebaceous environment of the hair follicle.
Malassezia folliculitis typically affects teenagers and young adults, presumably due to overactive sebaceous glands providing the perfect environment for the yeast to thrive.
Since Malassezia yeasts cannot grow without external lipids, they use the triglycerides found in human sebum as fuel.
The yeast would cleave host triglycerides into free fatty acids, which they then use to build their own mid-length and long-chain fatty acids to survive on.
The presence of the yeast in the follicle and the chemical compounds it produces trigger inflammatory responses by activating the complement system that includes macrophages, lymphocytes, and neutrophils.
The result of the inflammation is red itchy pustules and papules.
External Factors
Besides heavy and occlusive skincare products, environmental factors can also exacerbate fungal acne.
For example, Malassezia’s prevalence is highest in areas of high heat and humidity.
This condition coexists in 56% of acne patients in the Philippines, which probably has to do with the hot and humid environment.
Sweating is also often added as a factor that could potentially exacerbate fungal acne; however, sweat alone is unlikely to do this, as otherwise, we would probably be noticing fungal acne on the palms of our hands and soles of our feet where we tend to sweat a lot.
So, while sweating could potentially exacerbate the issue, it’s likely in areas where sweat is present alongside other components such as sebum.
How Does Accutane Work to Treat Fungal Acne?
Accutane is the brand name for the medication known as isotretinoin, an oral medication prescribed to treat severe acne.
It is commonly given to people whose acne has resisted previous treatments, such as benzoyl peroxide, adapalene, and antibiotics.
It has been observed that Accutane inhibits the function of the sebum-producing glands by reducing the gland’s size.
Therefore, since triglycerides in human sebum are essentially food for the Malassezia yeast, lack of it will cause the yeast to become starved, thus minimizing proliferation and eventually minimizing fungal acne, too.
How Long Does it Usually Take for Accutane to Clear Fungal Acne?
A study that consisted of six female adolescents with a combination of Malassezia folliculitis infection and acne vulgaris showed that Accutane resulted in a complete resolution of the inflammatory symptoms within three months of taking it.
This proves that Accutane can work for fungal acne; however, the medication is known to come with some unpleasant side effects, including:
- Excessive dryness.
- Peeling and shedding.
- Redness and irritation.
- Increased sun sensitivity.
- Joint pain in rare cases.
- Mood swings in rare cases.
Are There Any Other Treatments Available for Treating Fungal Acne Aside From Accutane?
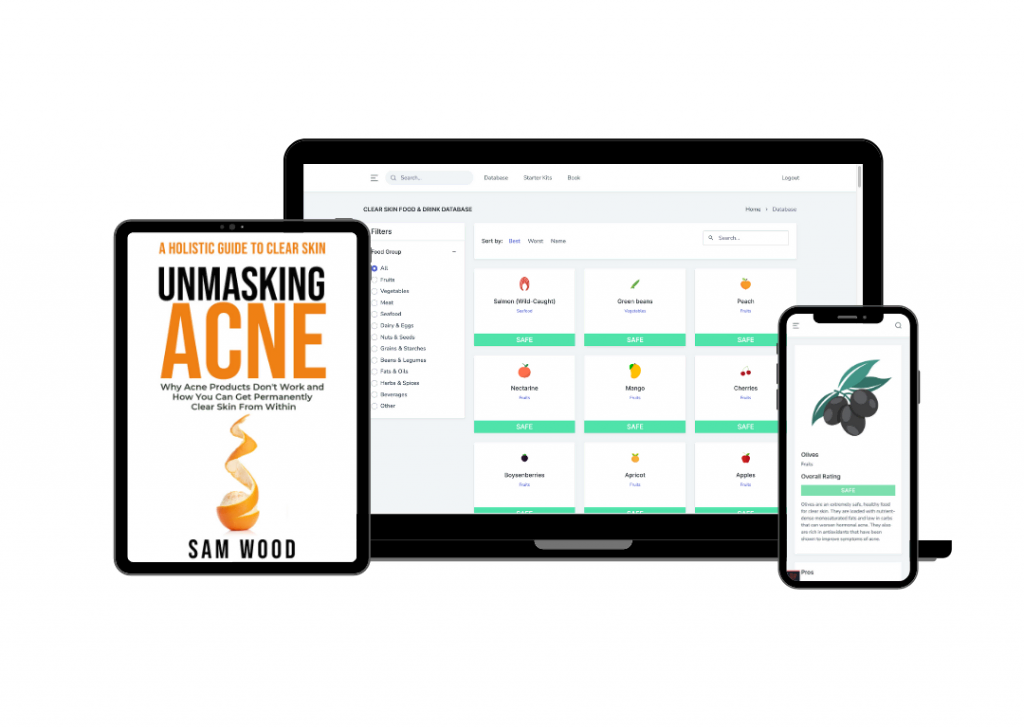
If you are a frequent reader of this blog you know we are big advocates of trying to improve your nutrition and lifestyle before trying out special soaps, moisturizers, medications, or other various types of medical procedures. We’ve had over 1,000 people to date clear their acne purely through nutrition using the Clear Skin Resource Kit.
However, at the end of the day, you need to wash your face. Fungal acne is unique because many common soaps actually make fungal acne worse. Several facial washes can help prevent the Malassezia yeasts through the use of Glycerin and several active ingredients listed below. This is why we created a detailed guide that gives our top recommendations for the best facial cleansers for fungal acne.
Ultimately, you should scrutinize all the cosmetics products you use if you suffer from fungal acne breakouts. The majority of primers, powders, and foundations will all exacerbate the spread of fungal acne because the oils, fats, and butters contained in many of these products help Malassezia yeast spread. Because of this, our team found several fungal-acne-safe makeup products that can be safely used on any skin type.
Trying out something milder and easily available is a good option before considering Accutane.
Here are some over-the-counter treatments that can help treat fungal acne:
Salicylic Acid
Salicylic acid is a keratolytic agent that can be an excellent treatment for fungal acne due to its anti-inflammatory, antibacterial, and anti-fungal properties.
Salicylic acid does a great job of dissolving cellular debris, including yeast overgrowth accumulated inside a clogged pore.
Retinoids
Retinoids are the topical and much milder version of Accutane. These are a class of chemical compounds derived from vitamin A used in dermatology to treat a wide range of pathogens, including bacteria, fungi, and viruses.
Multiple studies, both in vitro and in vivo, have demonstrated the efficacy of retinoids against a broad spectrum of opportunistic fungal pathogens found in human skin, including Malassezia yeasts.
And while you definitely need to do a bit of experimenting to find the right one for you, using an over-the-counter retinoid can help eliminate fungal acne.
Sulfur
Both cleansers and masks containing sulfur can be an effective treatment for fungal acne, even though they are only left on the skin for a short time.
Sulfur is naturally antibacterial and anti-fungal, allowing it to regulate fungal or yeast production and remove it from the clogged pores.
Over-The-Counter Ketoconazole
Some people have seen a drastic improvement in their fungal acne when using over-the-counter ketoconazole, an anti-fungal treatment found in up to 2% in shampoos like Nizoral.
However, this might not be the best option for everyone because shampoos also tend to contain silicones and other potentially-clogging ingredients, which may improve fungal acne due to the active ingredient but cause a bacterial issue down the line.
Not to mention shampoos can be too harsh for the skin on the face and shouldn’t be used too frequently as they can be extremely drying and irritating.
Best Prescriptions for Fungal Acne
When going the prescription route, you will likely be given antifungal medication that can be topical or oral to treat yeast overgrowth.
Topical antifungal therapy includes creams and lotions that contain:
- Econazole nitrate 1%.
- Clotrimazole 1%.
- Ciclopirox olamine 1%.
- Selenium sulfide 1% or 2.5% lotion used as a shampoo and body wash.
On the other hand, oral antifungal therapy will likely include:
- Fluconazole 100-200mg, taken daily for 2-3 weeks and then 200mg once a month for maintenance purposes.
- Itraconazole 200mg, taken daily for seven days and then 400mg once a month for maintenance purposes.
Are There any Natural Remedies That Can Help Treat Fungal Acne Effectively?
Fungal acne can definitely be a challenging condition to deal with.
However, besides many over-the-counter treatments and prescription options, you can also look into several natural remedies that can help treat fungal acne effectively:
Zinc
Zinc can be an effective treatment for fungal acne due to its ability to disrupt iron distribution across the yeast wall.
This action will effectively starve the yeast of the essential components it needs to thrive and proliferate and will reduce its overgrowth.
Witch Hazel
Witch hazel contains antioxidant components known as propyl gallates that protect human sebum from oxidation and stabilize the skin’s pH.
And since Malassezia needs oxidized sebum to thrive and proliferate, this action can reduce its overgrowth by providing an inadequate environment for the yeast to reside in.
Tea Tree Oil
Derived from the Melaleuca alternifolia plant, tea tree oil is a well-known antibacterial and anti-fungal component.
In vitro studies have also determined tea tree oil to be an effective component in inhibiting all yeast species, including Malassezia.
That being said, this potent ingredient shouldn’t be used directly on the skin without being diluted with a carrier oil such as jojoba prior to application, as it can potentially cause irritation and even a chemical burn.